 What are complementary and alternative treatments?
What are complementary and alternative treatments?
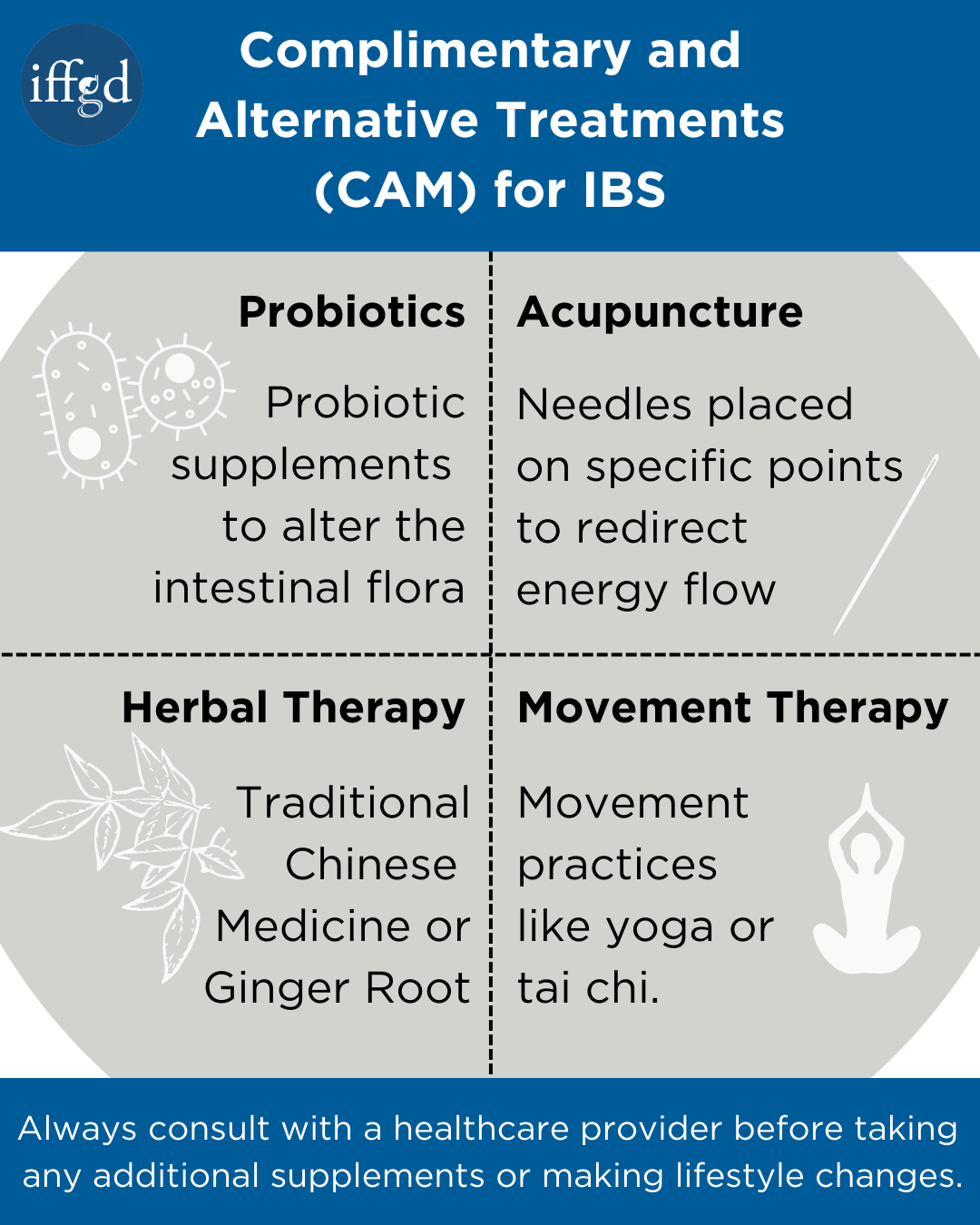
If conventional medical therapies prove unsuccessful or have unwanted side effects, many people choose to pursue complementary or alternative therapies (CAM). Complementary therapies are done in addition to traditional medical treatments, and alternative therapies are done instead of medical treatments.
Watch Dr. Anthony Lembo 2021 NES presentation Complementary Alternative Medicine CAM for GI Disorders to learn more about CAM.
Many complementary and alternative treatments modalities exist and they can be roughly grouped into several categories including herbal/dietary, somatic therapies (such as acupuncture or massage), mind-body therapies (such as hypnosis or meditation), and movement or breathing exercises (such as yoga or tai chi).
General safety advisory for consumers
- Before taking any supplement, herbal, or botanical, consult a healthcare provider or other health care provider – especially if you have a disease or medical condition, take any medications, are pregnant or nursing, or are planning to have an operation.
- Before treating a child with any supplement, herb, or botanical, consult with a healthcare provider or other health care provider.
- Like drugs, all supplements, herbals, and botanicals have chemical and biological activity. They may have side effects. They may interact with certain medications. These interactions can cause problems and can even be dangerous.
- If you have any unexpected reactions to a supplement, herbal, or botanical preparation, inform your healthcare provider or other health care provider.
For more information on dietary supplements, contact: Office of Dietary Supplements, National Institutes of Health, Web site: ods.od.nih.gov or, Center for Food Safety and Nutrition U.S. Food and Drug Administration, Web site: www.fda.gov/Food/default.htm
Herbal therapy
Herbal therapies have been used for a variety of disorders since ancient times. Traditional Chinese Medicine (TCM) has long used combination herbal therapy, which uses herbal formulas based on a patient’s pattern of symptoms, rather than a specific disease. Because of this, there is more than one formula for a disorder such as irritable bowel syndrome (IBS).
Herbs used in TCM formulas for IBS include many common foods such as rhubarb, barley, tangerine peel, cardamom, and licorice; and most formulas will include 5 or more herbs. While these therapies have been used in China for thousands of years, there has not been much research in the Western literature to assess their efficacy. One well-designed trial does exist which showed patients using herbal formulas had a greater improvement than those taking the placebo. This gives us hope that one day these TCM formulas might be shown to be helpful for IBS patients.
Sometimes individual herbs are used for specific gastrointestinal symptoms. Peppermint oil has been studied for use in both IBS and functional dyspepsia in capsule form. It is thought to act by decreasing muscle spasms in the gastrointestinal tract. Several small trials have shown that it is better than placebo in improving abdominal discomfort, bloating, or overall symptoms. Unfortunately, heartburn is a common side effect of peppermint oil treatment and it should be used with caution. Extensive reviews of the available trials using peppermint oil have determined that the data are insufficient to make clear recommendations for its use at this time.
Ginger is another common food product often used for gastrointestinal symptoms. Studies in IBS or dyspepsia have not been performed, but TCM practitioners, as well as many home remedies, often employ ginger. Ginger extract is thought to be anti-inflammatory, to strengthen the gastric lining, and to stimulate motility of the intestines. It has been shown to decrease nausea in several trials.
Unfortunately, although they are readily available without a prescription, clear safety and drug interaction information is unavailable on most herbal therapies. Always inform your healthcare provider about any herbal preparation you consider using.
Acupuncture
Acupuncture has its roots in ancient Chinese medicine but has become popular worldwide for many ailments. The basic theory underlying acupuncture is that there are channels of energy (Qi), called meridians, that run through the body. On the meridians are 360 acupuncture points. In a state of good health, energy flows freely on these channels. In disease, the energy flow is disrupted, leading to symptoms. Acupuncture to specific points is thought to release the energy and redirect its flow. In some cases, electrical stimuli are given to the acupuncture needles to increase the effect (electro-acupuncture).
Two very small trials examining acupuncture for the treatment of IBS have been performed with contradictory results. Despite this lack of data, many patients pursue acupuncture for abdominal pain, bloating, and nausea. Acupuncture is generally safe if performed by a licensed acupuncturist and maybe a good adjunct in patients who are sensitive or intolerant to oral medications. For severe cases, many acupuncturists will use acupuncture in conjunction with herbal therapy.
Alteration of the intestinal flora
Probiotics are substances or organisms that contribute to the balance of bacteria in the intestines. Probiotics are readily available in health food stores, and usually contain beneficial bacteria such as lactobacillus or bifidobacterium. The best evidence relates to a particular organism, Bifidobacterium infantis 35624. Studies have shown this strain to be superior to placebo in relieving the main symptoms of irritable bowel syndrome (abdominal pain/discomfort, distension/bloating, and difficult defecation).
Read more about probiotic treatments for IBS
Hypnotherapy
Hypnotherapy has been shown to be effective for IBS in several clinical trials. Hypnosis usually requires weekly individual sessions over several months but has been tried in groups and by self-instruction as well. Hypnosis involves progressive relaxation, then suggestions of soothing imagery and sensations focused on the individual’s symptoms. Improvements in overall well-being, quality of life, abdominal pain, constipation, and bloating have been noted.
One of the difficulties with hypnosis is that it is very dependent on the therapist, and it may be difficult to find a therapist both trained in hypnosis and knowledgeable about functional gastrointestinal disorders. Additionally, like many alternative therapies, it can be costly and often is not covered by insurance plans.
Read more about hypnosis treatment for IBS
Movement therapy and meditation
No studies on functional dyspepsia or IBS are available for specific movement therapies such as yoga or tai chi. It has been shown, however, that relaxation response meditation aids symptoms of abdominal pain, bloating, flatulence, and diarrhea. These types of therapies are particularly attractive, as they have no potential concerning side effects and may be helpful for symptoms outside the gastrointestinal tract, as well as promoting general stress reduction.
Conclusions
Complementary and alternative approaches to functional gastrointestinal disorders provide an exciting opportunity for both patients and healthcare providers faced with the difficulty of managing these chronic disorders. Currently, many questions about the efficacy and safety of CAM therapies still exist. More research into alternative therapies for functional gastrointestinal disorders is needed before definite recommendations can be made. It is important that CAM practitioners, primary care healthcare providers, and gastroenterologists work together with their patients to find the appropriate treatment or combination of treatments from the vast array of conventional and alternative options available.
Adapted from IFFGD Publication #181 by Kirsten Tillisch, MD and Steven Tan, MD, MTOM, LAc, Center for Neurovisceral Sciences and Women’s Health, David Geffen School of Medicine at UCLA, CA.
Additional Sources
NIH Office of Dietary Supplements (dietary-supplements.info.nih.gov) and FDA, Dietary Supplements (www.fda.gov/Food/DietarySupplements/default.htm)
