Sleep is an important part of a person’s overall health and wellness. Unfortunately, 40% of people with Irritable Bowel Syndrome (IBS) report having sleep problems. IBS symptoms, such as abdominal pain and diarrhea, can interrupt sleep patterns and consequently cause issues sleeping.
Sleep and IBS
There is little research on the link between sleep trouble and the gastrointestinal (GI) system. However, IBS has been linked with lower sleep quality, reduced light sleep, and significant sleep disturbance.
One study reports that IBS did not show any differences in areas such as total sleep time, time it takes to fall asleep, or amount of sleep in each stage. However, reported sleep trouble was more common in the IBS group. Additionally, a study that compared IBS patients to those without IBS showed that self-reported sleep trouble can be an indicator of “next-day” abdominal pain, anxiety and tiredness.
Learn More: Treating Pain in IBS
Other conditions affecting sleep quality and IBS symptoms
Sleep Apnea is a sleep disorder that affects roughly 20% of the population. Sleep apnea can interrupt sleeping patterns and lessen the quality of sleep. Common symptoms include snoring, witnessed temporary episodes of not breathing at night, and waking up with dry mouth. Researchers found that people with sleep apnea were more likely to have IBS than patients without sleep apnea. However, increasing severity of sleep apnea was not linked with IBS. These findings show the importance of following a treatment plan for diagnosed sleep apnea, and discussing symptoms with your healthcare provider to determine if testing for sleep apnea is necessary.
Mood disorders are commonly linked with IBS. Sleep trouble is a classic feature of psychiatric and mood disorders and likely play an important role in the link between sleep disturbance and IBS. Psychiatric include treatment and or conditions relating to the mind, behaviors and emotions. It is important to recognize uncontrolled psychiatric symptoms (nervousness, inability to focus, changes in mood, appetite, sleep) and discuss them with your healthcare provider.
Melatonin is a hormone produced by the brain that helps prompt sleep. A study looked at the effect of IBS patients taking melatonin supplements. This study showed that 3 mg of melatonin before bed decreased abdominal pain, but did not seem to improve sleep trouble. Another study found higher levels of melatonin in patients eating or drinking a probiotic. This research suggests that probiotics can alter the creation of melatonin through changes in gut bacteria. This can affect sleep and IBS symptoms. It is stressed that additional studies are needed as this is very early work. However, this will hopefully encourage further investigation into the link between IBS, the gut microbiome, and sleep
Tips to improve sleep:
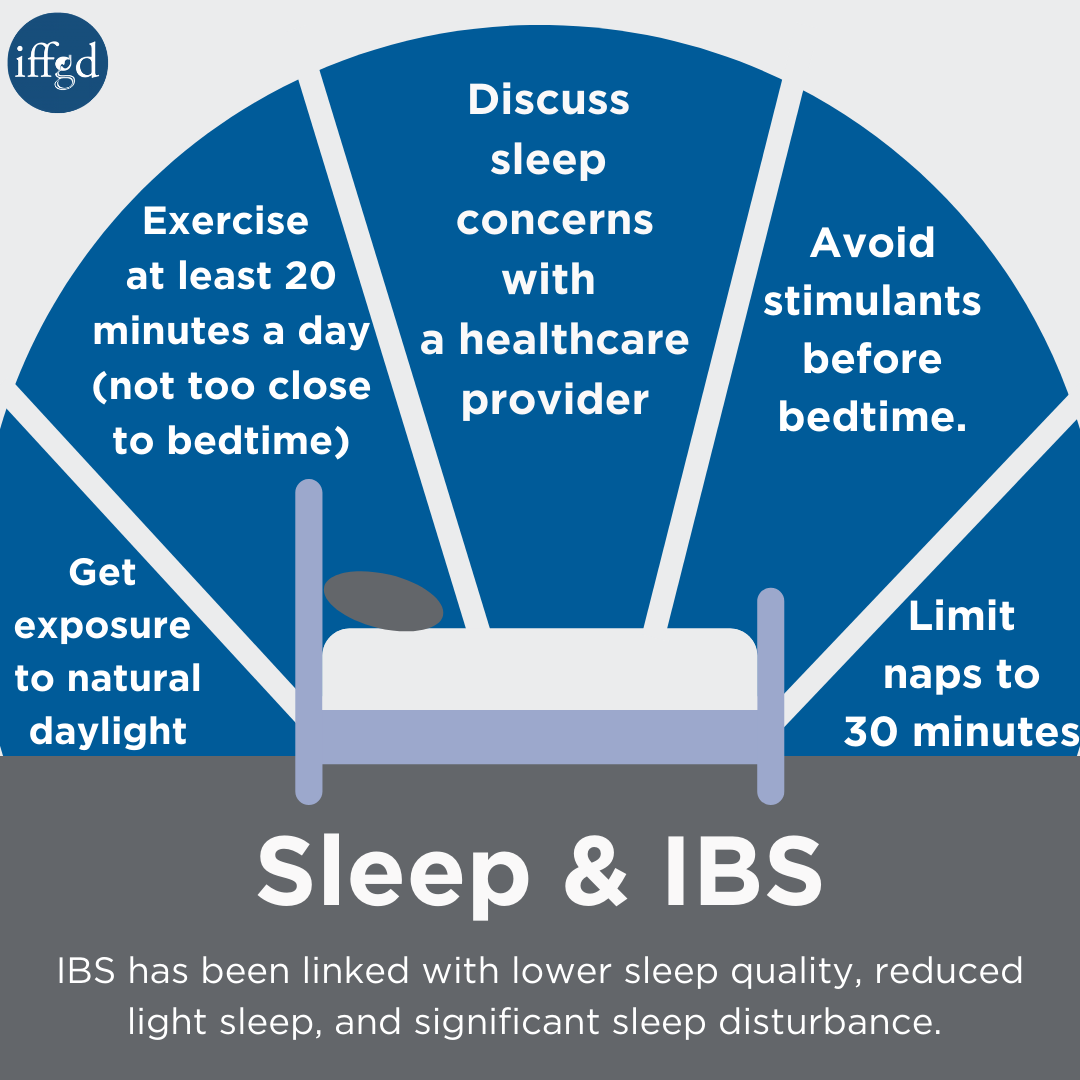
- Limit daytime naps to 30 minutes
- Avoid stimulants such as caffeine and nicotine close to bedtime.
- Exercise for at least 20 minutes per day- avoid activity in the few hours before bedtime.
- Get exposure to natural light during the day and darkness at night
- Optimize your sleep area by including comfortable bedding, “white noise”, blackout curtains, and avoid the use of electronic devices.
- If snoring or apnea (temporarily stop breathing) are witnessed, seek medical advice for further evaluation.
- Discuss sleep concerns with a healthcare provider including difficulty falling asleep or staying asleep.
- Discuss uncontrolled mood symptoms with your healthcare provider.
Unfortunately, it is safe to say that the average healthcare provider does not necessarily ask about sleep disturbance in patients with functional bowel disorders, and patients may not mention them to their treating healthcare provider.
Be sure to let your healthcare provider know if your IBS symptoms are disturbing your sleep. Treatment for sleep disturbance will likely improve your overall quality of life.
Summary
The above information highlights the link between IBS and sleep trouble. Sleep trouble in IBS patients is likely due to multiple causes, including changes in the sleep cycle, different views of sleep quality, and the presence of other medical problems linked with poor sleep (sleep apnea, mood disorders, etc.).
Although many questions remain unanswered at this time, it is reasonable to think that 1) IBS symptoms can cause poor sleep quality and 2) poor sleep quality can cause IBS symptoms. There is also growing evidence regarding the link of sleep trouble and changed pain view and visceral hypersensitivity.
If sleep troubles are experienced, it is important to discuss the sleep concerns with a healthcare provider. In addition to ruling out treatable conditions such as sleep apnea, healthcare providers can target therapies and recommendations to the identified sleep issue (i.e. trouble falling asleep, trouble staying asleep, trouble getting back to sleep after waking).
Adapted from IFFGD Publication #178 “Sleep and IBS” Written By: William C. Orr, Ph.D., President Emeritus, Lynn Health Sciences Institute; Clinical Professor, School of Medicine, University of Oklahoma Health Sciences Center; and National Sleep Foundation, Oklahoma City, OK Updated by: Kimberly Harer, MD ScM, Clinical Lecturer, University of Michigan, Ann Arbor, MI Edited by: Lin Chang, M.D., UCLA School of Medicine, Los Angeles









