Despite this, there are times when you have changes in IBS symptoms and it may be best for your healthcare provider to review your symptoms and how they affect you. Here are suggestions for when to seek additional guidance from a medical professional.
Developments of Concern
Wrong beliefs about IBS may lead to distress, more healthcare provider visits, and unneeded tests. It helps to know, IBS:
- Does not cause physical damage
- Does not increase the risk of colon cancer, inflammatory bowel disease (IBD), diverticulitis, or other gut disorders
On the other hand, IBS does not protect you from acquiring another disorder or condition. It also can coexist with another disorder.
Two situations provide alerts that another disease might be present:
- The presence of an “alarm” symptom or sign
- Clinical or family history linked to increased personal risk
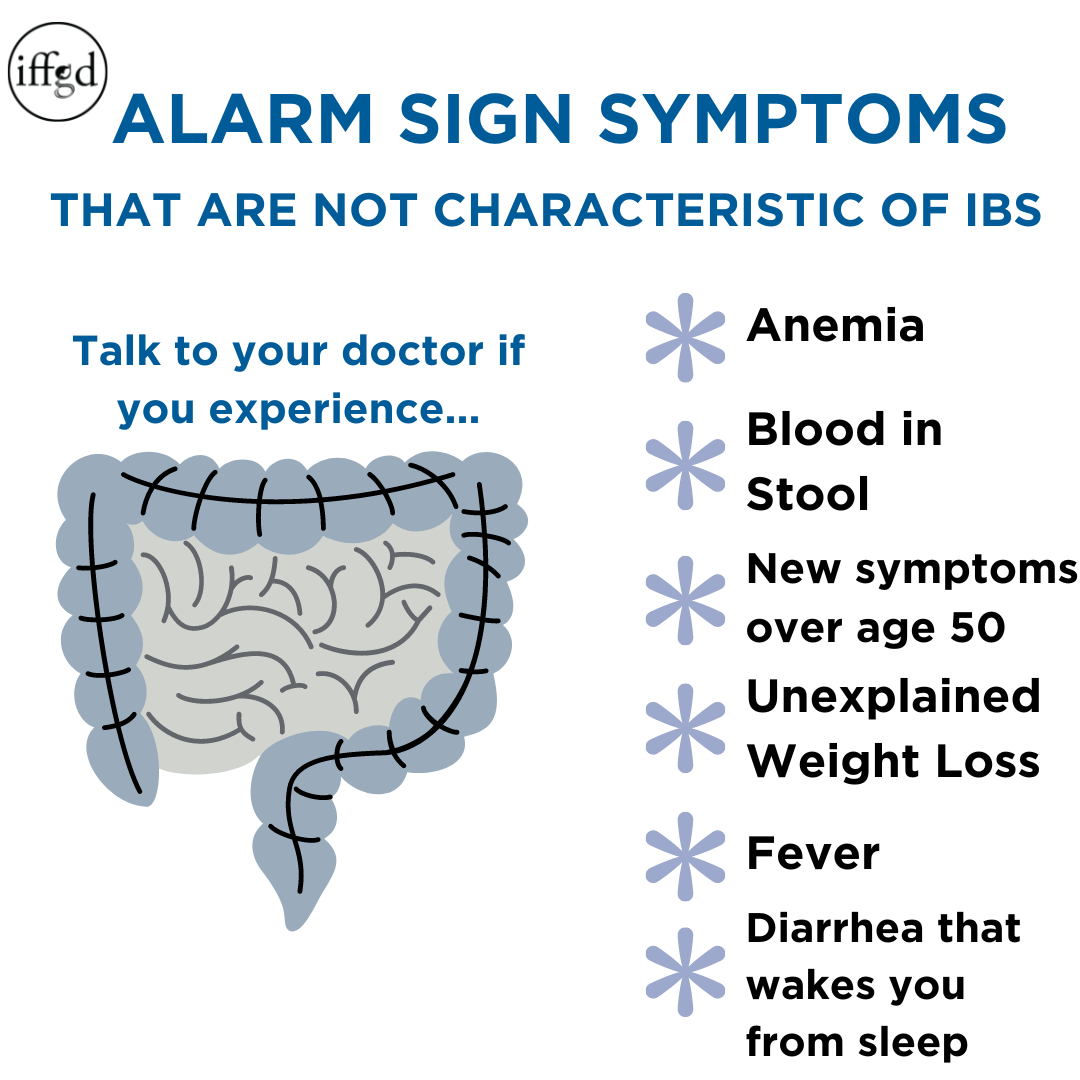
Changes in IBS Symptoms that are Alarm Symptoms
“Alarm” signs and symptoms are commonly called “red flags.” “Alarm” signs simply identify changes which are neither explained by nor consistent with a diagnosis of IBS. These require additional review by a healthcare provider. “Alarm” symptoms may be a sign of an underlying disease that physically damages the gut but may also be related to other conditions.
For example, rectal bleeding is one of the most alarming of such symptoms. This may be due to a hemorrhoid or small tear (fissure) in the anal canal. Bleeding through the rectum can also imply unhealthy changes or damage to the gut wall that should not be ignored. Sometimes it could be due to inflammation, a large polyp, or tumor which requires treatment. Large amounts of red blood or black, tarry stool calls for urgent medical attention. Tarry stool refers to stool the color of tar which is caused by bleeding in the upper GI tract.
There is a collection of symptoms that healthcare providers use to make sure something other than IBS is not causing symptoms. They are often called “Alarm signs” or “Alarm Symptoms”. These features include:
- New symptom onset at age of 50 or older
- Blood in the stools (red blood or black, tarry stool)
- Fever, shaking chills, or night sweats
- Nighttime symptoms that wake you up
- Unintentional weight loss
- Change in your typical IBS symptoms (like new and different pain)
- Recent use of antibiotics
- Family history of other GI diseases, like cancer, inflammatory bowel disease, or celiac disease
Learn more about alarm symptoms
Increased Personal Risk
Sometimes there is a factor in your life that may put you at greater than average risk of acquiring a serious intestinal disease. –Sometimes there are factors in your life that may put you at greater than average risk of developing an intestinal illness. Such examples are:
- Family history of chronic GI illness including cancer, Celiac, or IBD
- Sick contacts (e.g. family, friends, or co-workers) with recent intestinal illness
- Recent Travel: An infection may be suspected if you have recently traveled, had contact with others who are sick, or were possibly exposed to polluted water or food. Travel to the tropics or a developing country is a travel related risk factor.
- Antibiotic Use: Recent use of antibiotics or long hospital stays may increase the risk of an infection called C difficile. This infection typically appears with increasing abdominal pain and/or episodes of diarrhea (bloody or non bloody), nausea and/or vomiting. Sometimes fevers, chills, and sweats will occur as well.
IBS patients are as likely as anyone to suffer an intestinal infection, which may add to and confuse the symptoms. You should be suspicious of an infection if:
- You have been traveling to tropical or developing parts of the world
- Friends and family are infected
- You have been exposed to possibly contaminated drinking water
Let your healthcare provider know about any of these concerns.
When to See Your Healthcare Provider
IBS symptoms may be very hard to predict at first; however, over time most people become familiar with their symptoms. There may be intervals of relative calm, combined with periods of pain or discomfort. The flares may include chaotic bowel habits that interfere with daily life. However, the basic pattern of your symptoms should remain relatively stable.
If one of the previously described situations occurs or an alarm sign or new symptom emerges, it is time to see your healthcare provider. This allows them to decide if further testing or adjustments to your current IBS treatment is necessary. Sometimes a new drug or supplement may cause changes in symptoms. This is true even if they are not being taken for IBS. A change in your diet may also cause symptom changes, and your healthcare provider can help you make that determination.
Learn more about working with your healthcare provider
Putting it all Together
IBS is long-term (chronic) and tends to repeatedly come and go over time. It does not predispose you to other GI diseases. However, IBS does not protect you from other digestive conditions, and overlap is possible. New and different symptoms may make you suspicious that something new is happening.
You should visit your healthcare provider if you become aware of alarm symptoms or of a factor that might put you more than normally at risk of another disease. Your healthcare provider may review your symptoms and determine if further testing or treatment is necessary.
Usually, if the original diagnosis was sound, recurrent, but similar symptoms do not signify a new disease.
Adapted from IFFGD Publication: Changes You Should Not Ignore if You Have IBS Updated by: Walter Chan, MD, MPH, Director, Center for Gastrointestinal Motility, Assistant Professor, Harvard Medical School, Gastroenterology, Hepatology and Endoscopy, Boston, MA; Adapted from: W. Grant Thompson MD, FRCPC, FACG, Professor Emeritus, Faculty of Medicine, University of Ottawa, Ontario, Canada; Edited by: Darren Brenner, MD, Associate Professor of Medicine and Surgery, Northwestern University – Feinberg School of Medicine, Chicago, IL