The low FODMAP diet is not a “forever diet.”
The application of the low FODMAP diet requires the expert guidance of a Registered Dietitian trained in the area. It is very important to understand the Low FODMAP diet is done in 3 phases:
- Elimination phase
- Challenge phase
- Personalization Phase
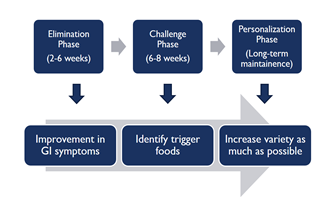
The goal of this approach is for you to figure out which FODMAPs you can tolerate, and which trigger your symptoms. This will help you best manage symptoms and eat a well-balanced diet with the most variety possible long-term.
When starting a low FODMAP Diet, Please Note:
- Not everyone feels better on a low FODMAP diet. If your symptoms do not improve on the elimination phase, you should add the high FODMAP foods you were avoiding back into your diet and consider other therapies available to improve symptoms.
- There is no benefit of avoiding high FODMAP foods unless they trigger your symptoms.
- To improve your odds of success, it is highly recommended to work with a Registered Dietitian (RD) with experience in teaching the low FODMAP diet.
- The low FODMAP diet is challenging and there is conflicting information online.
The Elimination Phase:
During the elimination phase, individuals will reduce or eliminate their intake of high FODMAP foods based on their dietitian’s recommendations with the goal of improving GI symptoms. This phase is usually 2-6 weeks but can vary based on a person’s needs. This phase involves identifying the foods that you are eating that are high in FODMAPs and swapping them with low FODMAP alternatives. During the elimination phase, your dietitian can help you identify which foods contain FODMAPs, and what you can eat, and ensure your diet stays balanced to help support your health and wellbeing.
The Challenge Phase
Once an individual sees improvement in their GI symptoms from the elimination phase, they can move on to the challenge phase. The challenge phase involves adding back in high FODMAP foods in a structured way to determine which foods and FODMAPs trigger symptoms and which do not. Some FODMAPs will cause symptoms to come back and some will not. Generally, a high FODMAP group or food is challenged one at a time for several days in a row. It is helpful to write down what you try, how much, and how you feel during this time.
Usually, one of three things may happen during a high FODMAP challenge:
- No symptoms will arise. This tells us that the particular high FODMAP food or group isn’t triggering GI symptoms and should be well tolerated moving forward.
- After challenging the FODMAP for a few days in a row, symptoms arise. This means small amounts of the FODMAP food or group are tolerated but portions may need to be limited or eaten less frequently instead of eaten every day.
- Symptoms come back immediately after challenging. This is considered a trigger and will likely need to be limited or avoided to improve GI symptoms. You can always go back and re-try a trigger in smaller amounts to see if this is better tolerated.
As stated before, if there are no improvements in symptoms during the elimination phase you should add all the high FODMAP foods back into your diet. Talk with your healthcare provider to find other potential therapies to aid in symptom improvement.
The Personalization Phase:
This can also be referred to as long-term maintenance phase. The goal during this phase is to increase variety and expand the diet as much as possible while continuing to minimize GI symptoms.
During the challenge phase, individuals learn which high FODMAPs trigger symptoms quickly, which FODMAPs can be consumed in moderation, and which FODMAPs are well tolerated. The high FODMAPs that are tolerated can be added back in the diet. It’s important to learn what alternatives you can add into your diet to replace the trigger foods that you are limiting/avoiding. Keep in mind that FODMAP tolerance can change over time. Individuals can always re-trial high FODMAPs that may have initially triggered symptoms.
Below is a sample menu choices guide for a low FODMAP diet (avoid using ingredients listed in the high-FODMAP food list)
| Breakfast | Gluten-free or spelt toast with spread (sucrose sweetened, not with fructose) Cereal (e.g. oats, Corn Flakes, Rice Krispies) Tea or coffee (if you have lactose malabsorption, use lactose-free milk) Serving of suitable fruit, Poached eggs and spinach |
| Lunch | Gluten-free or spelt sandwich with fillings (e.g meat, salad, cheese) Frittata Homemade soup with low FODMAP vegetables Green salad with dressing (olive oil, lemon juice) with tuna, Roast pumpkin, goats cheese & quinoa salad |
| Dinner | Meat or fish with low FODMAP vegetables or salad Baked fish with middle eastern vegetable quinoa Roast chicken with rosemary-infused vegetables and brown rice Gluten-free pizza base topped with cherry tomatoes, basil, goats cheese, ham, and pineapple |
| Snacks & Sweets | Serving of suitable fruit Yogurt (if you have lactose malabsorption, use lactose-free yogurt) Rice cakes with feta Gluten-free biscuits, Berry crumble |
Benefits of Working With FODMAP Trained Registered Dietitian
- They can ensure the low FODMAP diet is a good option for you given dietary restrictions, access to food/shopping, and nutritional needs. Some individuals may benefit from a modified version of the FODMAP diet or a different dietary approach altogether.
- They can make nutrition recommendations are tailored specifically to you.
- They will monitor to make sure you are getting adequate nutrients.
- They can provide you with up-to-date education on the diet and materials such as food lists and sample meals and snack ideas.
- They will focus on what to eat instead of only focusing on what to avoid.
- They can teach you to review product labels and find hidden sources of FODMAPs
- You will receive grocery shopping and dining out tips as well as cooking and recipe modifications.
- You will have access to an expert to answer your nutrition questions.
- You will get advice on next steps in case the low FODMAP diet doesn’t improve your GI symptoms.
Final Thoughts
A wide number of health benefits have been attributed to some FODMAPs. Fructans, inulin, and GOS are well-known prebiotics, stimulating the growth of beneficial bacteria in the gut.
For this reason, it is important to note that the “Low FODMAP diet” is not a “No FODMAP diet” and it is not a “lifetime diet.” We recommend that this diet is followed for 6–8 weeks and then your progress is reviewed by a dietician who will help advise which foods (and how much) can be gradually re-introduced into your diet.
Breath hydrogen tests are useful to identify which partly absorbed sugars – fructose, lactose, and the sugar polyols, behave as FODMAPs for the individual. (No breath tests are performed for fructans and GOS [galactooligosaccharides] since they will be malabsorbed in everyone.) For a minority of people (less than 2% of the community) who do not produce breath hydrogen or methane, breath tests do not provide useful information.
The dietician will also ensure that your diet is nutritionally adequate for you. Many people can return to their usual diet with just a few high FODMAP foods that need to be avoided.
For more information, visit http://www.med.monash.edu/cecs/gastro/fodmap/.
Adapted from IFFGD Publication #251 by CK Yao, Jessica Biesiekierski, Sue Shepherd, Peter Gibson, Eastern Health Clinical School, Monash University, Box Hill Hospital, Melbourne, Australia and Adapted from IFFGD Publication #117 FODMAP Overview by Emily Haller, MS, RDN, Registered Dietitian Nutritionist, Michigan Medicine, Division of Gastroenterology and Hepatology and Amanda Lynett, MS, RDN, Registered Dietitian Nutritionist, Michigan Medicine, Division of Gastroenterology and Hepatology. Edited by: Shanti Eswaran, MD, Associate Professor, Internal Medicine, Division of Gastroenterology, University of Michigan, Ann Arbor, MI
