
Functional gastrointestinal disorders (FGIDs), including IBS, are disorders of brain-gut interaction. This means that there is a problem with the way the central nervous system (the brain and spinal cord) and the enteric nervous system (the nervous system of the gut) communicate information back and forth about our digestion, appetite, thoughts, and emotions. The pathway between the brain and the gut is called the brain-gut axis, and it relies on chemical messengers, including serotonin, for communication. Indeed, 95% of your body’s serotonin, a neurotransmitter (chemical messenger) which is often known for its impact on mood, sleep, appetite, and sex drive, can be found in your gut! Thus, our emotional state is closely linked to the functioning of our gastrointestinal (GI) tract. In other words, the functioning of our GI tract affects our emotions, and our emotions affect the functioning of our GI tract (Figure 1).
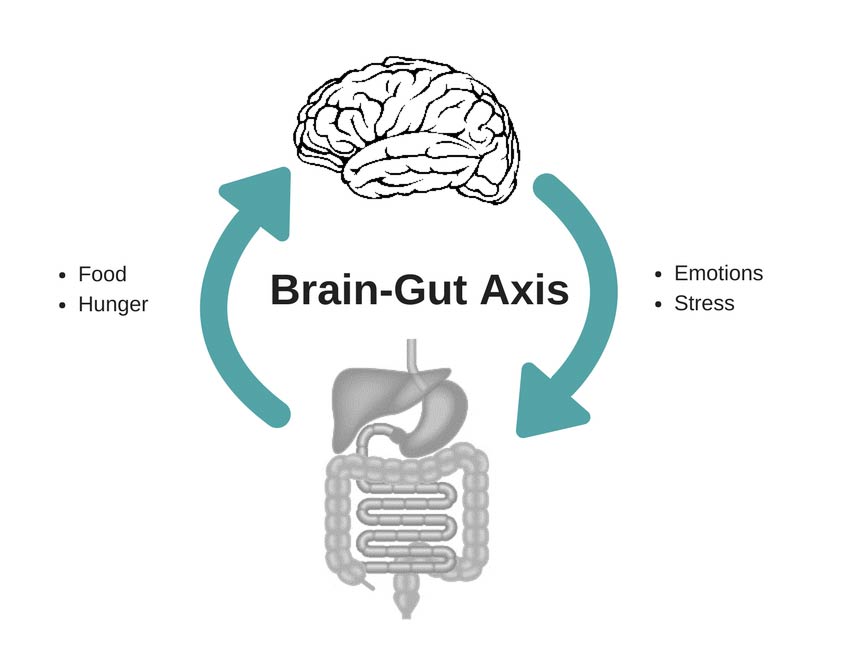
Figure 1 – The brain-gut axis
But My Symptoms are Real, Not in My Head!
Individuals with FGIDs are more likely than people without GI disorders to have depression and anxiety, although these can be seen as both risk factors for, and outcomes of, FGIDs. However, even for individuals with FGIDs who do not meet the criteria for a psychological disorder, fears, and worries that are related directly to their symptoms, known as symptom-specific anxiety, can contribute greatly to the severity of their symptoms. This is where cognitive behavioral therapy (CBT) can be a helpful tool to decrease GI symptoms and improve the overall quality of life.
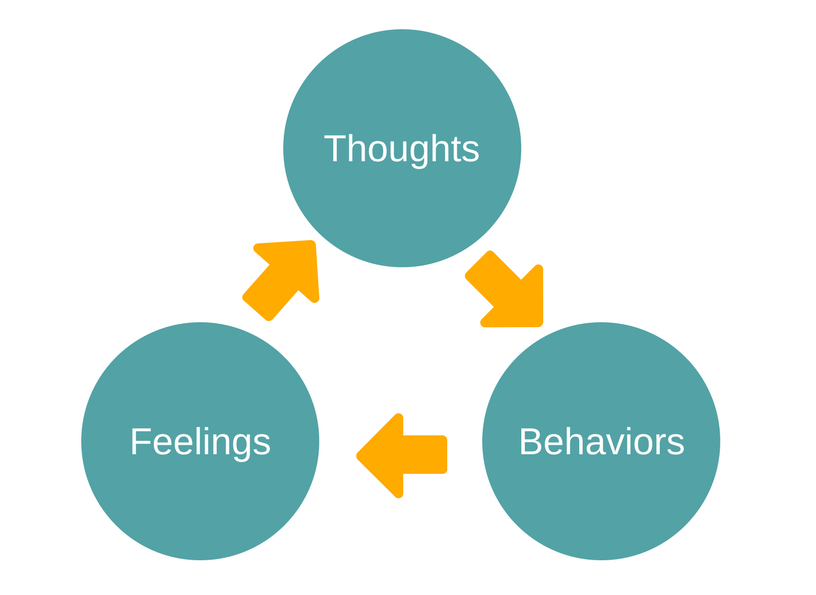
Figure 2 – The relationship between cognitions (thoughts), feelings, and behaviors.
Cognitive Behavioral Therapy (CBT)
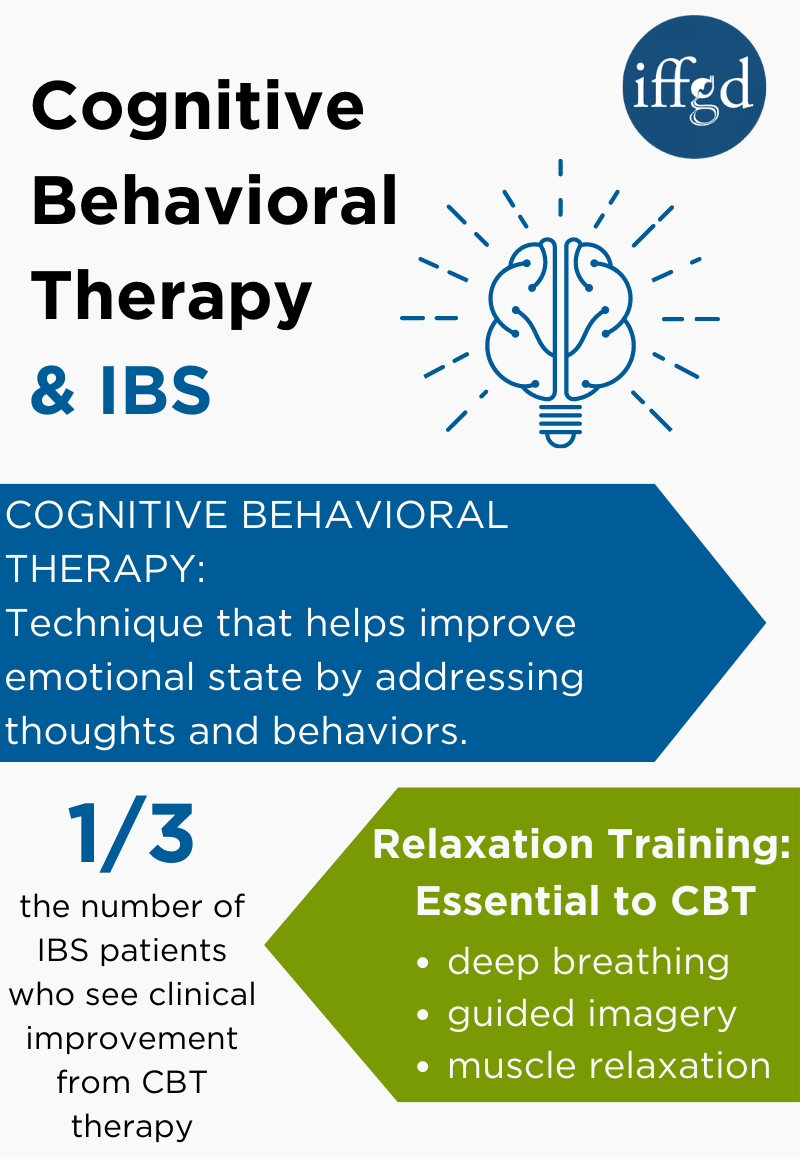 CBT is a type of psychotherapy originally developed and used to treat mental health issues, such as depression and anxiety. CBT is grounded in the belief that our thoughts (cognitions), feelings, and behaviors are all related (Figure 2). More specifically, unhelpful thoughts negatively impact how we feel and these negative feelings can impact how we behave. By evaluating and modifying our thoughts and behaviors to make them more helpful, we can improve our emotional state. CBT as a treatment tends to be short-term and collaborative. You and your therapist work together to make a game plan to address your symptoms, which typically includes both in-session and at-home practice.
CBT is a type of psychotherapy originally developed and used to treat mental health issues, such as depression and anxiety. CBT is grounded in the belief that our thoughts (cognitions), feelings, and behaviors are all related (Figure 2). More specifically, unhelpful thoughts negatively impact how we feel and these negative feelings can impact how we behave. By evaluating and modifying our thoughts and behaviors to make them more helpful, we can improve our emotional state. CBT as a treatment tends to be short-term and collaborative. You and your therapist work together to make a game plan to address your symptoms, which typically includes both in-session and at-home practice.
CBT can be used to stop the harmful effects of the fight or flight response by instead turning on the “rest and digest” response. Practicing deep breathing, muscle relaxation, and using guided imagery can all help move the body into this relaxed state. These methods are called relaxation training and are an essential component of CBT.
Fight or Flight Response
When a person experiences a symptom like pain, they may have negative throughts about the pain. Similar to fear or frustration, these negative emotions put the body into a “fight or flight” response, with an increase in stress hormones, blood pressure, and heart rate. Changes in the gut are part of this reaction to the danger that the body thinks it is facing and can include diarrhea, constipation, pain or discomfort.
Stressful events that are not an actual threat can also trigger the fight or flight response. For example, it is not uncommon for most people to experience abdominal pain when they are feeling nervous before speaking in front of a crowd.
Learn more about stress and IBS
Negative Perceptions
People who suffer with IBS might experience chronic pain or GI symptoms for years with no relief. Experiencing these chronic symptoms can impact the perception or view of what is happening. Over time, this distorted perception can worsen IBS symptoms. Below are two examples of distorted perceptions:
• Catastrophizing: The belief that something is worse than it actually is, dwelling on the worst aspects of a situation and thinking that one is helpless. E.g., “My stomach pain ruins everything!”
• Assuming the worst: Assuming we know the future and that the future is bleak. Sometimes it can be called mind-reading when we assume we know what others are thinking. E.g., “I passed gas in my exercise class, and now everyone thinks I’m gross.
These are just two examples of negative stories people tell themselves that can worsen symptoms. It is best to create a more positive mindset and consider how many things you can do, even when not feeling 100%. Also remember, people are not mind readers- they don’t always know what other people are thinking and making assumptions about it doesn’t help. Sometimes no one notices when we do something that we feel is obvious and embarrassing.
Stressful Events are Either Controllable or Uncontrollable
In life we experience all kinds of stressful events, both good and bad. Many stressful events can be seen either as controllable, which we can prepare for before or repaired after, or uncontrollable, or out of our hands. There are two approaches for coping with stressful events:
- problem-focused/active coping: focus our attention on addressing the problem, sometimes through pros and cons lists or action plans.
- emotion-focused/passive coping: Divert attention away from the problem and towards our own emotional state, which includes activities such as reaching out to friends and family or relaxation strategies.
Adaptive coping can help you choose the most effective coping strategy based on a stressor. Choosing problem-focused/active coping in the face of controllable stressors and emotion-focused/passive coping in the face of uncontrollable stressors is considered the most effective way to approach stressful events. CBT can help patients learn to adaptively cope with their symptoms by learning to strike the right balance.
How Do I Know This Works?
Research has shown CBT to be effective in improving bowel symptoms, psychological distress, and quality of life. A recent review and analysis of existing studies (meta-analysis) found that the number needed to treat for CBT in IBS is three, meaning that if three people are treated with CBT, one will clinically improve. This statistic is better than what is seen in several of the most effective FGID medications.
Determine if CBT helps relieve GI symptoms
The first step in learning about CBT is to make an appointment with a psychologist specializing in CBT and who has experience working with GI patients. After learning about a patient’s GI symptoms, mood, health, and stress levels, the psychologist will recommend whether CBT could be helpful in managing symptoms. The therapist collaborates with gastroenterologists and other health professionals. Patients typically meet with their therapists for four to ten sessions.
Adapted from IFFGD Publication #276: Cognitive Behavioral Therapy for IBS and Other FGIDs by Alyse Bedell, MS, Northwestern University Feinberg School of Medicine, and Laurie Keefer, PhD, Icahn School of Medicine, Mount Sinai, New York, NY. Adapted by Abigale Miller
Last modified September 2021
